Sight Stories
Restoring sight for all
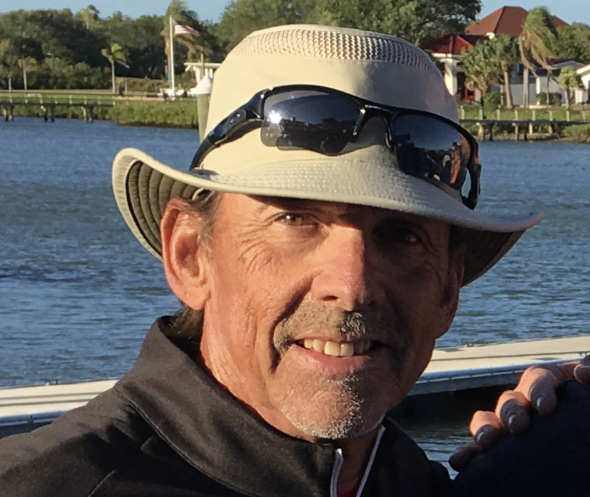
We are proud to share the stories of some of our patients who have experienced life-changing results from our services. These testimonials demonstrate the impact that our nonprofit has had on the lives of those we serve.
Inspired by these Stories?
We invite you to join us in our mission by supporting our nonprofit through donations or volunteering. Together, we can make a difference in the lives of those who need it most. Thank you for your support.